This post was published March 12, 2020 and has been updated frequently since then.
A friend of mine recently texted me in a fury.
“Someone just posted on FB that we’re doing things to stop the virus only because it’s going to ‘hurt old people’s feelings’ if we don’t,” he said.
His mother has respiratory issues and thus falls into the “older person vulnerable to the new coronavirus” category, as do many others.
Like me.
And I can read.
So when I read tweets or posts about how it’s basically “just a flu” (false) that “only hurts the vulnerable,” it makes me worry for us as a society. If we can’t protect our most vulnerable, what are we doing?
Don’t panic. Doctors/ virologists I’m speaking to say 98% of people will be fine, even if they get Covid-19. They expect it will go around the world, but that most people who get it will be a little sick, then recover. The danger is to vulnerable people. Hospitals/ old age homes.
— Richard Engel (@RichardEngel) February 26, 2020
COVID-19: We Need to Consider Society As a Whole
I’ve received many reader emails about COVID-19 asking for my thoughts given that I am currently dealing with a cerebrospinal fluid (CSF) leak and an inflammatory immune condition that already predisposes me to medication reactions and a cytokine storm.
It’s been very surreal to see the news unfold at a time when I have been in quarantine of sorts (bedrest) for many, many months. Due to the CSF leak, I rely on family and friends for groceries and to make food as I cannot do so myself. For those who are chronically ill, the lack of independence for basic needs adds an extra layer of concern and need for care on a daily basis.
The discourse about COVID-19 seems to consist of differing responses from several distinct groups of people
First, the people who are well and who believe they’ll be unscathed. This “isn’t a big deal,” they say. “Why is the media making us panic?”
Second, those who are vulnerable like me, and who know they are at risk for significant complications if they contract the virus.
There are some people who live in between those two extremes, and while healthy themselves are nonetheless able to remember a series of subclasses whose lives legitimately depend on the collective to stay safe.
And then, there are others whose actions are downright dangerous for all of us. This includes NBA player Rudy Gobert. Per Hot Air’s report:
I doubt we’ll get a better case study during this nightmare of how a single person’s cavalier denialism about the threat from the disease can put entire industries at risk. This happened two days ago. Gobert apparently thought it was silly that the NBA had set a new rule requiring reporters to stay six feet away from players at all time. So, as a goof, he decided to touch all of their microphones after his Q&A ended.
After mocking COVID-19 precautions by touching a bunch of things, he then tested positive. And as with any exponentially spreading virus, this exposure and infection have predictably led to others testing positive.
Jazz star Donovan Mitchell has tested positive for the coronavirus, league sources tell ESPN. Jazz players privately say that Rudy Gobert had been careless in the locker room touching other players and their belongings. Now a Jazz teammate has tested positive.
— Adrian Wojnarowski (@wojespn) March 12, 2020
Ultimately, Engel isn’t wrong from a statistical perspective.
He’s also not the first or last person I’ve seen try to stem the panic by reminding people of the expendability of the vulnerable like me.
I’m writing this post as a plea to each person to put overall societal needs above individual desires until this virus peaks and subsides.
I am not a doctor, and the following is not medical advice. It is, however, a summary of what I’ve researched for my own safety given my risk levels due to the issues with my immune system
Disinformation and panic don’t help anyone, especially during a pandemic.
By now, you’re probably living under a rock if your’e unaware of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), the artist formerly known as 2019-nCoV. SARS-CoV2 is the virus, and COVID-19 is the disease which that virus spreads.
People also refer to it as “coronavirus”, but since it’s one of many coronaviruses, I’m not going to do that here. MERS-CoV and SARS-CoV are two other coronaviruses you may have heard of. COVID-19 is a unique virus.
COVID-19 is a called Novel Coronavirus because it’s a new disease for humans. The World Health Organization estimates a global death rate of 3.4% of those who are infected. While many people around the world may have built up immunity to various flu strains over time, the newness of COVID-19 means no one had immunity to it when it first broke out. There is also no established treatment for COVID-19, and there is presently no way to cure it. There are some treatments in trial, however, and I’ve detailed them below.
The fast spread of this virus has led to heavy amounts of disinformation and even outright conspiracy theories. I’ve argued with quite a few people online who suggest that this is “just like the flu,” or that “most people barely feel sick.” In an internet age where we are able to quickly get data from countries that are ahead of our curve here in North America, there is simply no excuse for not acting as swiftly as possible.
Panic isn’t useful.
Changing nothing in your life isn’t useful either. It’s actually outright dangerous right now.
In the middle lies being informed, prepared, and willing to think about society as a whole. Doing so lowers the burden on our health care systems, and buys a bit more time for treatments and research to happen. Reducing the number of people who are sick at once is the best way to keep our health system from being overwhelmed. And that in turn helps not just COVID-19 patients but also everyone else who must seek treatment in a hospital.
Two factors that make COVID-19 a big concern to everyone:
- A medical system that is over capacity, where doctors will need to decide who coming in gets a ventilator, who gets a bed, and more – not just COVID-19 patients, but other vulnerable patients with chronic diseases. Data tracks at a 10% hospitalization rate in Italy for people infected with Covid-19, with those in critical condition needing 3-6 weeks for recovery. That puts a prolonged strain on the system.
- The lack of immunity to the disease worldwide means that there’s no ceiling on the amount of people who can get infected. Presently, cases of COVID-19 are doubling every few days. Research labs and scientists around the world are racing to find a vaccine that works, but as of today the only ways to address the outbreak are mitigation, and planning in an attempt to slow down the spread.
Asymptomatic carriers can help fuel a pandemic
Yes, the bulk of infections will be mild, per the available statistics we have.
But those mildly infected people can and will transmit this highly contagious disease to others. It is imperative that we keep the numbers low. At the beginning of COVID-19 coverage, news outlets reported that you were at risk of transmission if you had symptoms. As of mid-March 2020, however, studies are showing that even if you’re fully asymptomatic, you can still spread this virus as a vector.
For example, per CNN earlier in March 2020, Dr. Sandra Ciesek, director of the Institute of Medical Virology in Frankfurt, Germany, tested 24 passengers who had just flown in from Israel. Seven of the 24 passengers tested positive for coronavirus, despite four having no symptoms at all. Of great concern regarding the spread of this virus is that the viral loads for those four asymptomatic patients were actually higher than for the patients who exhibited symptoms. Viral load measures how concentrated a virus is in someone’s respiratory secretions, and a person with a higher load has a higher probability of spreading the virus to others
That is… not good.
The risk of transmission by people who seem healthy due to lack of symptoms is also contrary to what we were told initially, right? I know people keep saying that new information that they’re hearing about this virus contradicts what we’ve previously been told; but the reality remains that COVID-19 is a new virus that we are learning about globally, as the outbreaks continue.
Thanks to data shared from scientists in China and from doctors in Italy, South Korea, Singapore, and Taiwan, those of us ‘next in line’ — such as people in North America — are able to learn lessons from those other countries, and to model and see how we can adapt our protocols to this novel virus.
Joshua Weitz, a professor at Georgia Tech, co-authored a paper about the asymptomatic transmission of COVID-19, and published his takeaways in a mini tweet thread here. He urges everyone to practice social distancing now, to the extent possible. He notes that doing this reduces both your chances of getting sick and the chances of others getting sick because you can be “unknowingly ‘asymptomatic’ but infectious.”
Or, see the tweets from evolutionary biologist Benjamin Kerr below:
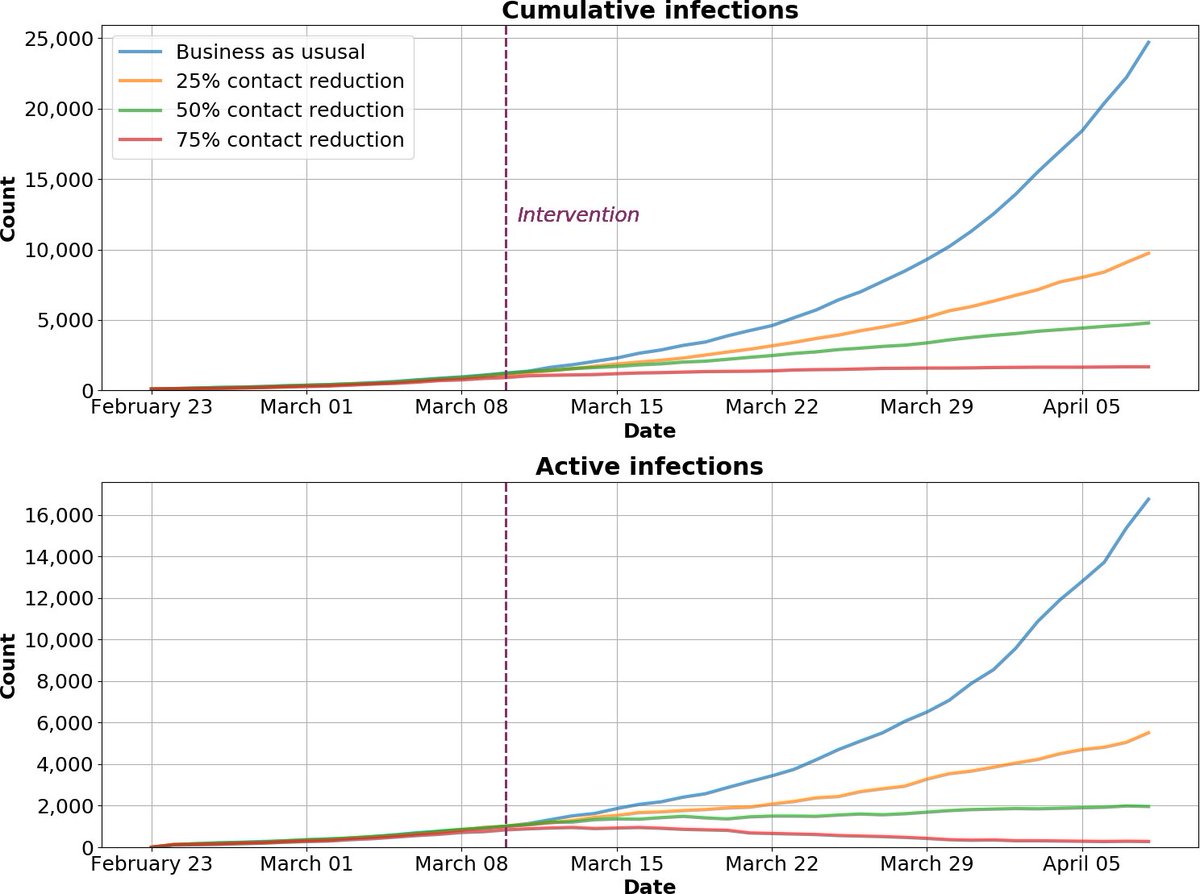
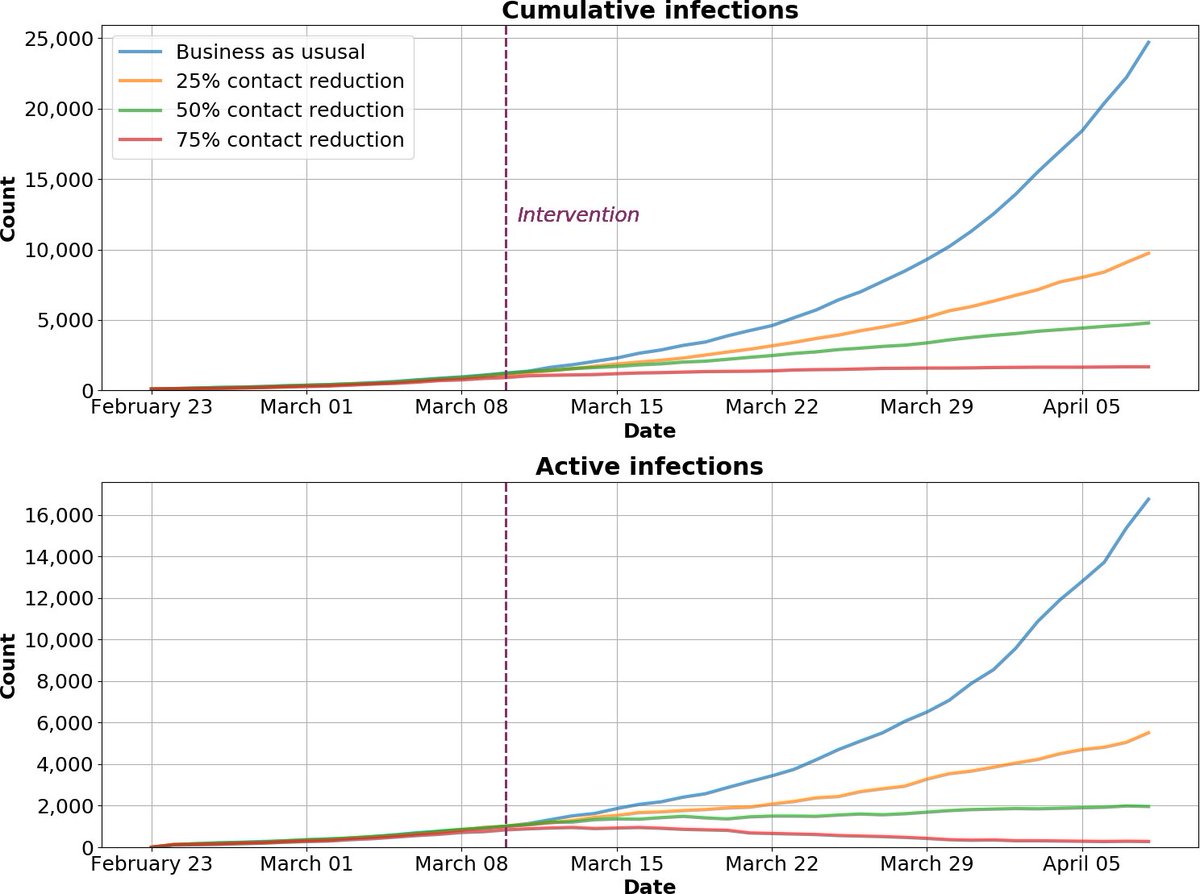
To illustrate the point, @ocornejoPopGen and I built a model (SEIR w/ high- & low-risk groups). Because low-risk people are more common, their behavioral change can have *greater* impact on lowering peak number of infections. Ideally, everyone limits interactions, but… [2/8] pic.twitter.com/5s5nxR0mZB
— Benjamin Kerr (@evokerr) March 14, 2020
(Full thread here.)
Which is why acting now, even if you’re healthy, is critical.
This also means preparing without panic, being reasonable about what we need and don’t need without hoarding, and above all considering our roles as citizens in a collective. As Mark Manson said in a new post:
So, while staying home, from an individual risk perspective, seems unnecessary and an overreaction, from a systemic risk perspective, it’s the only prudent thing to do. The more people who go out and about, the faster this thing spreads, and the faster this thing spreads, the more the hospitals get flooded, and the more the hospitals get flooded, the more people die unnecessarily.
Or, as Dr. David Juurlink, a physician at Toronto’s Sunnybrook Health Sciences Centre, says, “The faster this hits us, the less able we will be to provide care. The less able we are to provide care, the more people will die. It is as simple as that.”
This chart put together today by the Institute of Disease Prevention shows the potential mitigation of COVID-19 for King and Snohomish counties in Washington State by taking precautions sooner rather than later. The chart shows effects if people reduce contact with others by 75% vs. 50% vs 25% or .. nothing.
This virus is beyond containment worldwide, and acting swiftly but calmly is imperative.
Learning from Italy
Outside of mainland China, Italy now has the highest number of deaths in the world from COVID-19. And the country’s fatality rate from COVID-19—at 5%—is much higher than the global average of 3.4%.
US v Italy on #COVID19 cases. If the 17k positives we have today are the ONLY people positive and the growth rate continues at 35%/day (lower than this chart!) in two weeks 800k people will have it. In 4 weeks, 56 million. Let’s not assume we are immune to Italy’s probs. pic.twitter.com/EgoWSMFQDc
— Eli Pariser | @elipariser@mastodon.social (@elipariser) March 21, 2020
Why is Italy’s death rate so high? Italy has conducted a substantial number of tests — more than 42,000 as of Saturday (March 7), according to Al Jazeera. But the size of the outbreak and the late adoption of containment measures combined with speed of spread meant that Lombardy and to a lesser extent other areas in Italy are unable to get back to a place of balance. The strain on the system is so bad that the Italian College of Anesthesia, Analgesia, Resuscitation and Intensive Care (SIAARTI) has shared guidelines (link is in Italian) for the criteria that doctors and nurses should follow in these extraordinary circumstances, likening them to the moral choices doctors face during wartime. They require doctors to allocate ICU access to the patients with the highest chance of therapeutic success. This may seem logical and even utilitarian, but it’s a devastating position to be in every day during an outbreak.
At the same time, an Italian doctor begged other countries to act now. Dr. Daniele Macchini posted (link is in Italian; English here) about what’s happening on the front lines of Italian’s coronavirus response, noting that each ventilator was like gold and that many of the doctors were themselves getting sick with the virus. He notes that there are no more specialist doctors, just doctors as a whole, a single team to try and stop the inflow of sick people. Italy does have a sizeable older population, but the case study of Dr Macchini and others on the front lines would be foolish to ignore.
The foregoing is not “media hype” but rather published testimony and guidelines from a country right in the middle of a substantial outbreak. Most Western countries are on a similar trajectory as Italy, with a time delay. From March 14th:


We need to think through the exponential growth of this disease, and we don’t seem to be doing so on a systemic level. The way exponential growth works is that it seems tolerable until suddenly it’s an avalanche – and then it’s often too late.
Let’s try to avoid the avalanche.
Risk Groups for COVID-19
Briefly, because we’ve all been bombarded with graphs these days, a note about mortality and risk groups.
The CDC has released the following guidance for pre-existing conditions that are known to be factors in worsening COVID-19 infections in patients, in a Community Mitigation Strategy document:


The medical consensus is that those over 60 years old, and those with the conditions above, are most at risk.
In addition to the main pre-existing conditions listed above, immunocompromised patients are at higher risk for fatalities. And there are millions of immunocompromised people in America alone, a number which not only comprises those with immunodeficiency syndromes but also people with cancer (who are accounted for in the above chart), or who have been treated for it, people who have received transplants, people with HIV, and more.
For those who fall in the vulnerable class of patients, extra precaution is needed. What is also needed — as this post will keep saying over and over — is for everyone to take social distancing seriously, especially because of testing limitations in many countries but especially the United States.
It’s NOT just the elderly
While the bulk of fatal infections have shown to strike those in advanced years and/or those who have the pre-existing conditions referenced above, this does not mean that if you’re young you’re all good. In the United States, we are learning, young people are hospitalized in large numbers. CDC data shows that nearly 40% of patients sick enough to be hospitalized were between 20 to 54 years old. And in a system that risks being overwhelmed, every hospital bed counts. All the more reason to self-isolate now.
ProPublica interviewed a respiratory therapist in New Orleans (article not for the faint of heart), and noted:
Since last week, he’s been running ventilators for the sickest COVID-19 patients. Many are relatively young, in their 40s and 50s, and have minimal, if any, preexisting conditions in their charts. He is overwhelmed, stunned by the manifestation of the infection, both its speed and intensity.
Stay. Home. Now.
Symptoms of COVID-19
The symptoms of Covid-19 vary from case to case. From China’s data, the most common are:
- fever
- dry cough (majority of cases)
- fatigue
- mucus coughing up from the respiratory tract (called sputum)
If you have a fever and dry cough alone, advice from interviewed doctors is to get tested by calling your department of health – NOT by presenting to the ER or Urgent Care where you could potentially infect others.
“We really want to raise awareness that this is a sign of infection and that anyone who develops loss of sense of smell should self-isolate,” Prof. Claire Hopkins, president of the British Rhinological Society, noted to the New York Times on March 22, 2020.
:no_upscale()/cdn.vox-cdn.com/uploads/chorus_asset/file/19782405/Coronavirus_Symptoms___WHO_joint_mission_2.png)
Contacting your Department of Health for your state, province, or territory is a starting open, since many have opened Coronavirus Hotlines to help direct you appropriately toward testing.
- For Americans: state department of health contact information here.
- For Canadians, scroll down to the phone numbers of each provincial health department, here.
Also call your GP or primary care doctor if you have one, as well as local hospitals, if there is no hotline or dedicated response from your local Department of Health.
And – it goes without saying but here we go: STAY HOME unless advised otherwise by one of the hotlines or medical professionals in your life.
Are there any treatments for COVID-19?
No drugs or biologics have been proven to be effective for the prevention or treatment of COVID-19. But, numerous antiviral agents, immunotherapies, and vaccines are being investigated and developed as potential therapies.
In trials/studies to ascertain whether it could work for COVID-19:
Genetic Engineering and Biotech News summarizes the 60 current treatments under investigation for COVID-19, including potential vaccines in development.
Where testing comes in
Data from Italy suggests that many cases went undetected and enabled community spread. This data is part of why it is extremely important to get testing capacity up to population numbers, and why containment in the USA is going to be a big problem.
As of late-March 2020, it’s still difficult to get tested in the USA.
There continues to be widespread confusion about #COVID19 testing. One problem is that there are so many different roadblocks that have slowed things down–even when earlier ones are cleared, new ones have popped up. Testing has scaled up, but it’s not enough yet. 1/x
— Suzy Khimm (@SuzyKhimm) March 13, 2020
Several Legal Nomads readers in the USA have reported symptoms consistent with COVID-19, obtained doctors’ requests for testing, and still were told by the Departments of Health in their states that they were not eligible for testing. New York State has now begun testing widely and as a result has more COVID-19 cases than France or South Korea. As of March 22, 2020, New York State had tested 61,000 people. Other states will hopefully follow suit.
Those readers did the smart thing and put themselves on self-quarantine, but what of the many potentially infected people who did not?
Based on exported cases to other countries, Italy may have had about 4000 #COVID19 cases by end of Feb, rather than the 1100 that were reported, suggesting about 70% of cases went undetected. More great analysis by @AshTuite and co https://t.co/CI4dENGlyr
— Adam Kucharski (@AdamJKucharski) March 6, 2020
Strain on the hospital system when catastrophe medicine is at play, especially in the USA
The facts for the US health care system during this pandemic are not great.
According to the American Hospital Association, as of 2017, the US had 924,107 beds total. On a per capita basis, that was 2.77 beds per 1000 people. For comparison, China’s 2017 per capita bed ratio was 4.05 beds per 1000 people. (See OECD healthhcare stats here.)
Put simply, there are not enough hospital beds in the USA for an outbreak of the kind we’ve seen elsewhere, nor for the projection of hospitalizations – 4 to 8 million – that researchers estimate the United States will see. In fact, the US’s ratio of hospital beds per 1000 people is also smaller than those of the other main countries overwhelmed with outbreaks of this virus. The respective ratios for Italy and South Korea as of 2017 were 3.18 and 12.27.
Moreover, with at-will employment in many states and many employees receiving few sick days — especially in jobs that are front-facing (service industry, food industry, etc.) — increased community spread is likely.
And then there are patients who are chronically ill and depend on medication and hospital needs even outside the “at-risk” aspect of COVID-19. If the system is overwhelmed as we’ve seen happen elsewhere, deaths from pre-existing conditions that can’t get properly treated are more likely.
From a family friend, a doctor in Indiana who reviewed the Indiana State Department of Health Crisis Standard for Ventilator Allocation:
Here’s the problem: If we can’t find a way to slow the spread of this virus in the United States, the healthcare system will be faced with a surge of patients that may overcome available healthcare resources. Things like ventilators and ICU beds may be inadequate.
But most patients survive, right? The flu kills more people, right? Well, that’s again not the whole truth. Take a look at the news out of Italy. Hospitals are overrun at 200% capacity. They have ICU patients in operating rooms. They have run out of ventilators. Patients are being triaged into likely to survive or not likely to survive. The former receive a ventilator. The latter receive oxygen and medications to keep them comfortable as they die. That’s because this virus is capable of making people – especially older people and people with comorbid conditions – very very ill. None of us have immunity to this illness, and unlike flu none of us have been vaccinated against COVID-19. If this illness is allowed to spread unchecked, far too many patients will require care at the same time forcing doctors and hospitals to choose between patients who are likely to survive and those who are not – a process called ventilator allocation.
Oh come on, isn’t it just like the flu?
No.
For the love of all things holy, NO.
This isn’t the flu – it’s a different virus altogether. Scientists in Asia have described it as a cross between SARS and AIDS in terms of how it impacts the body.
It is more contagious than the flu.
It is more deadly than the flu.
Even assuming a global death rate of 1% (despite the current death rate of 3.4-3.5% of infected people per the WHO), it would be 10 times more deadly than the flu, which has a death rate of 0.1%.


The data from all around the world indicates a much higher mortality rate and a very different virus altogether from seasonal influenza. China’s datasets, as well as those from countries like Taiwan and Singapore where so far containment has been possible, have all provided us with information to help us see what’s coming.
Won’t it go away when temperatures rise?
We don’t know. This virus is so new that we just don’t know yet. We know that COVID-19 is an “envelope” virus, meaning that it’s packaged not only in a capsid protein, but also in a membrane (the envelope), usually made of lipids. Soap’s effectiveness at breaking down these lipids when people wash their hands properly is part of why the “wash your hands!” instructions are being shouted from every rooftop.
This envelope interacts with our cells during infection, and helps the virus dodge attempts to eradicate it from the body. Generally speaking, viruses with envelopes are more fragile and vulnerable to adverse conditions, says Neal Nathanson, an emeritus virologist at the University of Pennsylvania Perelman School of Medicine.
In a 2010 paper “Absolute Humidity and the Seasonal Onset of Influenza in the Continental United States,” scientists posited that a drop in in absolute humidity was far more relevant to the flu’s ability to replicate than temperature or general humidity in the air. But why that is we just don’t know. One of the authors of that paper, climate geophysicist Jeffrey Shaman, confirms in a Science Magazine piece that yes, lower absolute humidity might favor some viruses. But the why remains unclear.
“Variables that could affect the viability of the viral membrane could include changes in osmotic pressure, evaporation rates, and pH, Shaman says. “Once you get down to the brass tacks of it, we don’t have an answer.”
I mention seasonality because quite a few people have brought that up as an argument not to worry now. “Oh, it’ll go away in the summer,” they’ve said.
We just don’t know that. And even if it does go away in warmer, more humid places, it may roar back just like the 1918 influenza did. So slowing the curve down to make sure our hospitals don’t get overwhelmed remains important.
So what are the projections for infected people within the United States?
Per a New York Times article updated March 18th:
“Between 160 million and 214 million people in the United States could be infected over the course of the epidemic, according to one projection. That could last months or even over a year, with infections concentrated in shorter periods, staggered across time in different communities, experts said. As many as 200,000 to 1.7 million people could die.”
Those worst-case assumptions, however, do not take into account the mitigation measures that are now swiftly being put in place by states, cities, businesses, and individuals. As I’ll explain below, social distancing really is helpful in slowing down the strain on the system, and ensuring that the sick get the care they need to lower the chances of them being casualties.
People who are usually reasonable and rational are nonetheless comparing this virus erroneously to the flu or saying it’s just overblown hype. This is not only unkind, to belittle someone’s fears about their own health and safety, but negligent for the wellness of society.
Please don’t make fun of people who are scared of this very real threat, especially if they’re in the vulnerable class.
Please don’t downplay actual data and case reports from around the world where doctors have been fighting this virus to the point of exhaustion.
The success of our outcome depends on individual willingness to mitigate risk moment to moment.
So what can we do? Think collectively, not individually, to help flatten the curve of the epidemic.
“We are past the point of containment,” says @UWMedicine Dr. Helen Chu. “Now we need to keep the people who are vulnerable from getting sick.” #COVID19seattle
@UWVirology @WADeptHealth WADeptHealth @KCPubHealth https://t.co/q4mvKarU2D— UW Medicine Newsroom (@uwmnewsroom) March 6, 2020
Those who require hospitalization require the long term stays of ICU care that I mentioned earlier, for a period of 3-6 weeks. Italy thus far estimates that many COVID-19 patients need at least 4 weeks on mechanical ventilators.
That number would put hospital systems over capacity very quickly if we don’t flatten the curve on this virus.
:no_upscale()/cdn.vox-cdn.com/uploads/chorus_asset/file/19780273/flattening_the_curve_final.jpg)
:no_upscale()/cdn.vox-cdn.com/uploads/chorus_asset/file/19780273/flattening_the_curve_final.jpg)
This virus is going to affect your life. And you get to decide if you want to contribute to flattening the curve, or spiking it.
I sound like a broken record for social distancing because we know testing isn’t going to get everyone and thus if we want to have a bell curve more like South Korea versus like Italy, we need to start taking action on an individual level yesterday.
I realize not everyone has the privilege to work from home or to take all the measures I list below.
But doing as much as possible is extremely important for EVERYONE, in order to help ease the impact of this pandemic.
“When people change their behavior,” said Johns Hopkins associate professor Lauren Gardner in the New York Times, “those model parameters [i.e., the worst-case scenario numbers cited above] are no longer applicable . . . There is a lot of room for improvement if we act appropriately.”
Fine, you’ve convinced me. Now how do I help stop the spread for COVID-19?
Starting place: do not panic.
Each of us thinks better and makes smarter decisions when we are not in cognitive overload. The earlier you take precautions, even if you’re not directly impacted yet by the virus, the better you can help lower the societal burden. Choose compassion for the societal burden over fear and distrust. I know it’s not easy, but as a collective we do depend on it.
Worldwide data shows there is no advantage to being a late mover here. As the WHO director general, Dr. Tedros Adhanom Ghebreyesus, said on March 13th, all possible action should be taken. “Not testing alone. Not contact tracing alone. Not quarantine alone. Not social distancing alone,” he said. “Do it all.”
1. SOCIAL DISTANCING
Does your company let you work from home? Start doing so now.
Limit nonessential public gatherings.
Make small choices that can take away from groups of people, even in quotidian activities. Refrain from museums, clubs, dancing, religious services, and more as this plays out. Crowded spots are prime dissemination spots.
What is a “public gathering”? Doctors I have spoken with define a public gathering as anything more than 6 people, but there doesn’t seem to be consensus overall as you can see with the number (5) below. Regardless of the actual numbers, social distancing is how we can have a hope at slowing the spread of COVID-19, and potentially mitigate its effects on the hospital system. The Atlantic has a “DOs and DON’Ts of Social Distancing” piece from March 12th here.
The same doctor in Indiana who wrote about ventilator allocation above, says:
This means not flying on a plane or taking a cruise or a train. This means cancelling your vacation. This means not going to gatherings of people. How many is too many people? To give you an idea, one of the health organizations I work for has banned meetings of more than 5 people. Most meetings are video or teleconferenced. So should you go to a crowded school event or a sporting event? NO! And schools shouldn’t be so irresponsible to continue to offer such gatherings.
This also includes cancelling non-critical medical visits, to keep the hospitals and systems as clear as possible for the coming burden. Telemedicine has been available for a few years now, and this is definitely the time to avail yourself of it if you have the privilege to do so.
I’ve been telling people, “be St. Louis, not Philadelphia,” because in 1918, Philly held a huge parade during an influenza outbreak. In contrast, St. Louis cancelled all gatherings. As you can see from the chart below, the death toll was very different in those two cities.
There is a reason for canceling public gatherings. In a pandemic, don’t be Philadelphia (held a parade in 1918 when cases started to come up, downplayed cases), be St. Louis (canceled gatherings). More here: https://t.co/KE7RYbxDGM @mlipsitch pic.twitter.com/wyrHx0nOLA
— Florian Krammer (@florian_krammer) March 6, 2020
It’s selfish to complain about “changing your plans” or making adjustments to social activity when the downside of doing nothing is systemic overload and catastrophe medicine.
It should go without saying, but do NOT fly on a plane if you’re awaiting COVID-19 results. A passenger from New York to West Palm Beach, Florida did just that.
Again, this isn’t hype, this is simply a summary of what we’ve seen in other countries to date with medical systems that don’t have enough beds for contagion at this volume.
People like me don’t have the privilege to be out in the world safely right now, and nor do your parents and grandparents.
2. WASH YOUR HANDS. OFTEN. LONGER THAN YOU WANT TO.
The most important thing other than social distancing is to wash your hands, for 20 seconds.
That’s a lot longer than most of us are accustomed to taking when we wash our hands. And we need to do it frequently. Before and after eating food. When returning home from outside. When in contact with anyone else. If there is a chance your unwashed fingers have the virus on them, you do not want them anywhere near your face (see below), nor do you want them touching surfaces in your home
“Happy Birthday” sung twice is about the right length, so many people are singing that as they wash. Here’s a song generator from The Verge that can help you choose other options so you don’t hate birthdays by the end of this COVID-19 pandemic.
If Neil Diamond is your jam, he has generously released a special edition of ‘Sweet Caroline’ specifically for COVID-19 hand-washing, called ‘Hands Washing Hands’:

Soap works very well on this virus, and it doesn’t need to be anti-bacterial soap. It just needs to be a looooong wash, because of the nature of the virus.
For the science behind why that is, see the thread below:
1/25 Part 1 – Why does soap work so well on the SARS-CoV-2, the coronavirus and indeed most viruses? Because it is a self-assembled nanoparticle in which the weakest link is the lipid (fatty) bilayer. A two part thread about soap, viruses and supramolecular chemistry #COVID19 pic.twitter.com/OCwqPjO5Ht
— Palli Thordarson (@PalliThordarson) March 8, 2020
If you cannot use soap and water because you’re away from access to them, alcohol-based hand sanitizer with over 60% alcohol content is a good stand in. When you do get access to soap and water, though, wash immediately.
3. STOP TOUCHING YOUR FACE
THIS IS SO HARD.
I’m not alone; a study from 2015 shows people touch their faces an average of 23 times per hour.
It’s very important though, and we have to keep avoiding it as much as possible. This includes the eyes, since ocular transmission has been one of the ways the virus is spread.
4. DISPOSABLE GLOVES IN CERTAIN SITUATIONS.
Wear nitrile or latex disposable gloves when in public spaces like buses, subways, and other areas where you will be touching areas that others have touched like pumping gas.
If you are in a social situation where you need to remove your gloves, do not touch your face or eyes, no matter how much something itches. And before you put gloves back on, wash your hands thoroughly with soap and warm water, scrubbing the fingers.
If you don’t have gloves but are using light switches, elevators, or other public buttons or switches, use your elbow to hit the button instead of your hand.
As with everything involving a virus this contagious, it’s extremely important to discard your gloves safely. The CDC has a PDF on how to dispose of contaminated gloves safely from its Ebola guidance, here.
5. STAY 2m (6 FT) AWAY FROM SICK PEOPLE, AND TRY TO KEEP DISTANCE OF 1m (3 FT) GENERALLY WHEN OUTSIDE.
This means life changes that have irritated some people, but nonetheless are reasonable precautions during an outbreak like this.
And still, social distancing takes precedence.
Netflix instead of a movie theatre. There’s even a Chrome Extension called Netflix Party that allows you to watch as a group while chatting with friends. If you’re want to dine out, there are ways to keep distance. Either get take-out food and bring it home, or sit outside if there is a terrace instead of staying inside a closed restaurant. You get the drill.
Serious Eats has a Comprehensive Food Safety and Coronavirus primer from the exceptional J. Kenji López-Alt*, who discusses all things food, including special precautions restaurant owners, kitchen managers, or other folks with food-related businesses should be taking. He also gets into the safest ways to shop at grocery stores or supermarkets. Worth a bookmark.
Some further advice for safely receiving food delivery: pay the entire amount, not just the tip, online or over the phone in advance (since cash is an effective medium for transmitting viruses); ask for food to be left outside your door instead of actually interacting with the deliverer; use your own pen if you’re signing for the food in person; and transfer the food to your own dishes before eating.
*Kenji’s book is one of my favourite cookbooks. He is presently donating 100% of his sales commissions towards producing food to be served free of charge to needy families and individuals affected by school and business shut-downs in San Mateo, an additional 10% of the sale cost will go to a nationwide network of independent bookstores.
6. THIS MEANS NO HAND SHAKING OR CHEEK KISSING TO GREET PEOPLE. OR ELBOW BUMPING, DESPITE THE POPULARITY OF THAT GESTURE AS A SUBSTITUTE
Curtsy, briefly bow, bring your hands together as if in prayer, nod your head with a smile at someone — these are just a few options or just do a head nod with a smile.
No hand shaking or cheek kissing for greetings as they bring you too close.
According to the WHO, no elbow bumping either as it also brings you into contact:
❌ No handshakes, no kissing, not even elbow-bumping.
How do you greet people during a #coronavirus outbreak? The WHO’s @DrTedros recommends contact-free way. More @business: https://t.co/jw8XtgvFHw #COVID2019 pic.twitter.com/RclX8TusuZ
— Bloomberg Quicktake (@Quicktake) March 12, 2020
7. AVOID PUBLIC TRANSPORTATION AS MUCH AS YOU CAN.
This likely doesn’t require an explanation, but is to avoid a cough, sneeze, or hand-to-hand contact that can put us in the danger zone for droplet splatter or air particles that can transmit the virus.
8. DOORKNOBS: LEARN TO CLEAN THEM OFTEN AND TRY NOT TO USE THEM IN PUBLIC.
I’m very limited here because of my CSF leak, but for those of you who can open and close doors using your elbows, hips, or shoulders: do it. If not, wear gloves to turn a doorknob, or wash your hands immediately after touching it. If someone does get sick in your household, wiping down your doorknobs is a good idea too.
A March 17, 2020 study notes that “SARS-CoV-2 was more stable on plastic and stainless steel than on copper and cardboard, and viable virus was detected up to 72 hours after application to these surfaces.”
The CDC has a list of cleaning recommendations for COVID-19 (which notes that the virus can survive on some surfaces for days) here.
9. WIPE DOWN YOUR CELL PHONE WHEN YOU RETURN HOME FROM OUTSIDE.
I use alcohol-wipes for this, small size, but the ones I bought are no longer available. A spray bottle with rubbing alcohol sprayed onto a wipe will usually suffice. Apple used to say not to clean phones this way, but due to COVID-19, Apple has changed its guidelines. The company now says you can use a wipe with 70% isopropyl alcohol or a Clorox wipe to clean your iPhones. For non-Apple devices, see this piece from CNET.
10. WHEN THE WEATHER ALLOWS, OPEN A WINDOW.
This virus cannot linger in a well-ventilated space, per this FP article, though it’s quite cold in much of North America still.
11. ON MASKS
There is a lot of controversy about masks. If you do choose to use one, you need to don and doff it with gloves on, and then make sure you properly dispose of the gloves.
When the mask has been taken off, place it inside of a disposable container or bag, seal it, and put it in the trash.
In a March 12th piece, The Guardian recommends wearing masks when caring for sick people and when around sick people:
Wearing a face mask is certainly not an iron-clad guarantee that you won’t get sick – viruses can also transmit through the eyes and tiny viral particles, known as aerosols, can penetrate masks.
However, masks are effective at capturing droplets, which is a main transmission route of coronavirus, and some studies have estimated a roughly fivefold protection versus no barrier alone (although others have found lower levels of effectiveness).
If you are likely to be in close contact with someone infected, a mask cuts the chance of the disease being passed on. If you’re showing symptoms of coronavirus, or have been diagnosed, wearing a mask can also protect others. So masks are crucial for health and social care workers looking after patients and are also recommended for family members who need to care for someone who is ill – ideally both the patient and carer should have a mask.
However, masks will probably make little difference if you’re just walking around town or taking a bus so there is no need to bulk-buy a huge supply.
If someone is coughing or sneezing it’s good to ask them to put on a mask to protect you.
The guidelines from China, Hong Kong, and Japan do suggest wearing masks, and while surgical masks will not protect you 100% from the virus there is reason to don one if you have them available. Priority remains that medical providers have sufficient masks and gloves to wear. If in North America and Europe we are able to access them without shortages to critical care personnel, then they might be a good idea.
The Czech Republic has made them mandatory, already, and people are sewing them across the country:
This is one of the most amazing and hopeful things I’ve read. How the Czech Republic, through community effort, got to 100% mask usage in 10 days, nearly all thru home DIY effort.
They only have 2 deaths and have no growth in daily new covid-19 cases.https://t.co/xsS4POZUs9 pic.twitter.com/9nAGCfjipt
— Jeremy Howard (@jeremyphoward) March 24, 2020
If you’re in North America, Speakeasy Travel Supply company is currently sewing masks on a donation basis, here.
12. DON’T FORGET TO STAY SOCIAL, EVEN INSIDE
I’ve been on bedrest now for close to two years, and with technology I’ve been able to keep myself sane and connected with friends. In times like this, where fear often takes over, it’s even more important to stay in touch with people you love even if you can’t see them.
An epidemic of loneliness is not what does the immune system good. These are three things that really helped me during bedrest and isolation the last few years:
- I scheduled nighttime calls with friends to calm myself before bed.
- I watched Netflix programmes with friends and family in faraway places, with each of us pressing “play” at the same time.
- I started meditations in groups every Sunday for 10 weeks, where we all meditated to the same track at the same time. At the peak of these sessions, we had hundreds participating and it was delightful.
I found that connecting to others was the most helpful way to keep my spirit high, and it also gave me ample time to catch up with people I loved who I had not spoken with in years. Video calls on FaceTime or Skype kicked it up a notch and gave me even more smiles.
Plus, many companies and cultural institutions have begun streaming such content as video recordings of operas, Broadway shows, and ballets; virtual tours of museums from around the world; films that normally are unavailable online, including movies that had been scheduled to screen at festivals that have been cancelled, and more.
Kudos to all the cultural outlets who are streaming performances and screenings for #FlattenTheCurve shut-ins. I’m going to start aggregating the ones I see below, starting w this from the Met. https://t.co/kwJ1cNtjoC
— Garance Franke-Ruta (@thegarance) March 14, 2020
The bottom line is to find a way to be a part of the human experience as a whole, even if you’re stuck inside.
Or if you’re in a city, do as residents of various Italian cities have done and start a massive singalong with your neighbours from your window or balcony:
https://twitter.com/leonardocarella/status/1238511612270690305
12. STOCK UP, RESPONSIBLY
Make a list of crucial prescription medication as well as over-the-counter medication such as and cold/pain relief, and stock up for a month’s extra supply – or more if your insurance allows.
In Canada, most people I’ve spoken with have gotten 2 months’ extra supply of prescription medication when they refilled their prescriptions. In the USA, this will vary by state and insurance provider.
Examine also has a list of immune-supporting supplements that may be of interest, including Vitamin C and Vitamin D (the latter of which has been shown to help with respiratory infections in studies).
Other things to have in the house:
- All-purpose cleaner
- Hand soap
- Dish soap
- Rubbing alcohol in case you need to dilute it to make a spray.
- Paper towels
- Cold & flu medicine that you favour, if any.
- Painkillers like Tylenol or Advil
- Latex gloves or nitrile gloves to wear donning and doffing masks, or for use outside the home.
- Toilet paper (for a few weeks extra not a panicked buy of a monster load of toilet paper!)
- Bleach or Lysol or Clorox Wipes for cleaning.
- Toothpaste
- Laundry detergent
Some non-perishables that are easy to have in case you want to minimize your food trips: rice, canned tuna or chicken, protein bars, popcorn, crackers, nutritious seeds like flax or chia, peanut butter, oats, cans of chickpeas and beans, and oils you use to cook with. Also some frozen veggies.
Don’t forget the pets! Stock up on pet food for an extra month.
How long will the COVID-19 outbreak last?
We don’t know yet. But experts like Michael Osterholm, who appeared on MSNBC in a MSNBC on March 15, 2020 video interview, are approaching the coronavirus outbreak “like a Minneapolis blizzard, where if we just hunker down for a couple days … we’ll get through. This is really much more like a coronavirus winter.”
In the UK, Public Health England documents accessed by The Guardian note that the outbreak is expected to last until Spring 2021.
The vulnerable are worthy of protection too.
On March 12th, Norway instituted a mandatory quarantine for all inbound travelers and cancelled classes at all schools, as well as all sporting events. They also have a mandatory quarantine for people coming into the country from abroad.
In the USA and Canada, many of these large-scale domestic measures have not happened yet, though more and more cancellations are happening each day.
We know that the countries that have been most successful at lowering their overall death rate are the ones that take swift, aggressive measures quickly.
In South Korea, for example, nearly 20,000 people are being tested every day for the virus and labs are working 24/7 to get testing kits processed. This morning, I heard a segment on NPR from a man there who tested positive despite his only symptom being a slight cough. In Seoul, the radio anchor reported drive-through testing with results delivered via text in 5-6 hours.
Taiwan, too, has tested every resident with unexplained flu-like symptoms for COVID-19 since January 31, 2020, and tests every traveler with fever or respiratory symptoms. Taiwan has had only one death from COVID-19 so far. Moreover, in addition to proactive testing, the government acted swiftly with crisis management tools, combatted misinformation, and focused on resource management throughout.
We can see from Italy what happens when we don’t take a preemptive, wide-reaching approach. Let’s not squander the horrifying lesson they taught us. It’s clear that the US does not have the capacity to test at high levels like South Korea, meaning many people who are otherwise asymptomatic could be infecting the vulnerable classes in society.
It took me many days to write this article because I can only stand for small 20-minute increments to write it with my CSF leak. But it’s well worth the “up time” if it makes a few more people take COVID-19 seriously.
Stay home.
Do what you can to protect the at-risk population.
Change your schedule, your patterns, your habits to the maximum extent you can.
Just because I’m vulnerable to this virus doesn’t mean I’m less worthy of staying well.
COVID-19 Resources

